Similarities and Differences between Flu and COVID-19
November 28, 2022What is the difference between Influenza (Flu) and COVID-19?
Influenza (flu) and COVID-19 are both contagious respiratory illnesses, but they are caused by different viruses. COVID-19 is caused by infection with a coronavirus (SARS-CoV-2) first identified in 2019. Flu is caused by infection with a flu virus (influenza viruses).
From what we know, COVID-19 spreads more easily than flu. Efforts to maximize the proportion of people in the United States who are up to date with their COVID-19 vaccines remain critical to reducing the risk of severe COVID-19 illness and death. More information is available about COVID-19 vaccines and how well they work.
Compared with flu, COVID-19 can cause more severe illness in some people. Compared to people with flu, people infected with COVID-19 may take longer to show symptoms and may be contagious for longer periods of time.
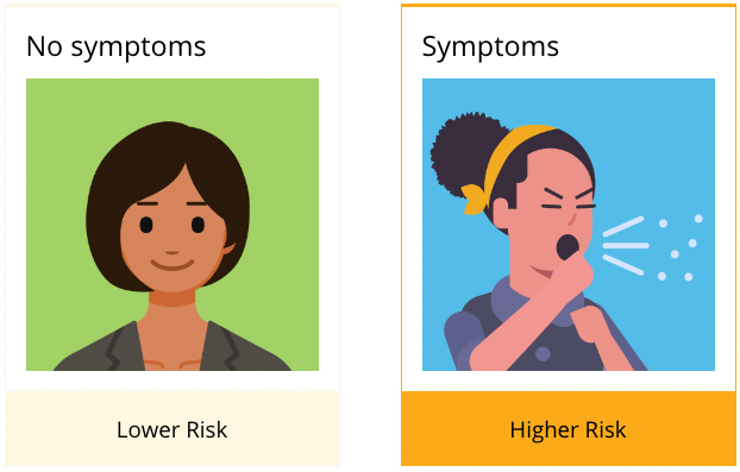
You cannot tell the difference between flu and COVID-19 by the symptoms alone because they have some of the same signs and symptoms. Specific testing is needed to tell what the illness is and to confirm a diagnosis. Having a medical professional administer a specific test that detects both flu and COVID-19 allows you to get diagnosed and treated for the specific virus you have more quickly. Getting treated early for COVID-19 and flu can reduce your risk of getting very sick. Testing can also reveal if someone has both flu and COVID-19 at the same time, although this is uncommon. People with flu and COVID-19 at the same time can have more severe disease than people with either flu or COVID-19 alone. Additionally, some people with COVID-19 may also be affected by post-COVID conditions (also known as long COVID).
We are learning more everyday about COVID-19 and the virus that causes it. This page compares COVID-19 and flu, given the best available information to date.
Similarities:
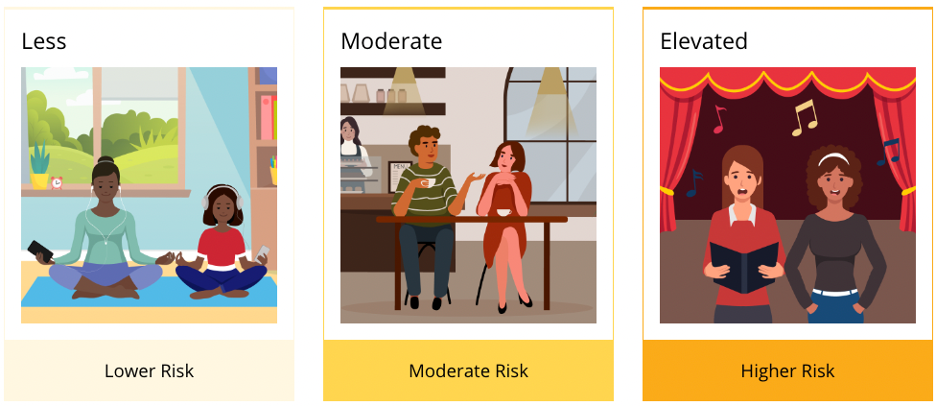
Both COVID-19 and flu can have varying degrees of symptoms, ranging from no symptoms (asymptomatic) to severe symptoms. Common symptoms that COVID-19 and flu share include:
- Fever or feeling feverish/having chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue (tiredness)
- Sore throat
- Runny or stuffy nose
- Muscle pain or body aches
- Headache
- Vomiting
- Diarrhea (more frequent in children with flu, but can occur in any age with COVID-19)
- Change in or loss of taste or smell, although this is more frequent with COVID-19.
Differences:
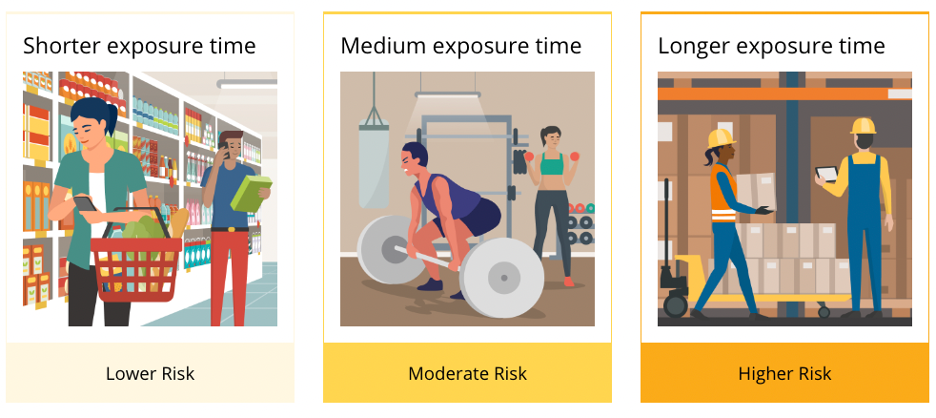
If a person has COVID-19, they could be contagious for a longer time than if they have flu.
Flu
- People with flu virus infection are potentially contagious for about one day before they show symptoms. However, it is believed that flu is spread mainly by people who are symptomatic with flu virus infection.
- Older children and adults with flu appear to be most contagious during the first 3-4 days of their illness, but some people might remain contagious for slightly longer periods.
- Infants and people with weakened immune systems can be contagious for even longer.
COVID-19
- On average, people can begin spreading the virus that causes COVID-19 2-3 days before their symptoms begin, but infectiousness peaks one day before their symptoms begin.
- People can also spread the virus that causes COVID-19 without experiencing any symptoms.
- On average, people are considered contagious for about eight days after their symptoms began.
To learn more, please visit https://www.cdc.gov/flu/symptoms/flu-vs-covid19.htm.