Providing Care to a Diverse Older Adult Population
April 22, 2024Your patients bring diverse backgrounds, customs, abilities, and experiences to their health care. Some differences are apparent, while others are not. Factors that contribute to diversity include:
- Geographic and cultural background
- Race and ethnicity
- Age
- Gender identity, gender expression, and sexual orientation
- Preferred language(s)
- Religious and family traditions
- Education and socioeconomic background
- Neurodiversity
- Cognitive, sensory, and physical abilities
Recognizing and appreciating diversity is an essential part of patient-centered care. It can lead to improved patient safety, more open communication, increased health equity, and better patient outcomes. By respecting each patient’s values and preferences, you’ll be more likely to engage them as collaborative partners in their care.
How is diversity related to health?
A patient’s culture and background will affect whether and where they seek health care, their understanding of medical information, and how they make health care decisions. Recognizing the different health issues your older patients are likely to face, as well as the factors that contribute to these differences, will help you provide the most effective care.
Many complex and interacting factors, lifelong and current, underlie disparities in health risk and disease burden. These factors include:
- Unequal access to health care services
- Availability of social support
- Neighborhood and workplace environments
- Food availability and accessibility
- Wealth and income gaps
- Racism, sexism, and other forms of discrimination
Age-related health disparities affect the health of older adults. For example:
- NIA-funded researchers have found a higher prevalence of Alzheimer’s disease among African Americans and Hispanics than among other racial and ethnic groups in the United States.
- Prostate cancer has higher incidence and mortality rates, as well as an earlier average age of onset, in non-Hispanic Black men compared with men of other backgrounds.
Scientists have also observed sex and gender differences in health and longevity. For example, women live longer than men, on average. They are also more likely to develop osteoporosis or depressive symptoms and to report functional limitations as they age. Men, on the other hand, are more likely to develop heart disease, cancer, or diabetes.
Other studies have found that lower socioeconomic status is associated with poorer health and reduced lifespan in the United States. Economic circumstances can determine whether an individual can afford quality health care and proper nutrition from early life into old age. Financial resources and health insurance often determine whether an older adult enters an assisted living facility or nursing home or stays at home to be cared for by family members.
Health care workforce diversity is important
Providers representing a variety of backgrounds and cultures can help meet the health needs of an increasingly diverse population. Some patients feel more comfortable with health care providers who share or understand their language, race, ethnicity, or other cultural characteristics. Research suggests that a diverse health care workforce may also improve patient satisfaction, patient-clinician communication, and access to care.
Communicating with a diverse patient population
Your conversational style can be a subtle but powerful way to connect with your patients. Being thoughtful about how you communicate with each individual can promote understanding, trust, and satisfaction in the patient-provider relationship.
Practical tips for effective communication include:
- Ask patients which name and other descriptive terms they prefer and use those consistently. This small effort can go a long way toward making patients feel welcome, safe, and accepted.
- Use person-first language. This language avoids defining someone by their condition or disability (e.g., people with diabetes instead of diabetics).
- Try to match your communication style to that of your patient. Conventions such as the speed and volume of speech vary across cultures. To some people, interrupting an individual who is speaking is acceptable and even expected, while it is considered rude and off-putting to others.
- Use plain language. Avoid using medical terminology or abbreviations that your patients might not understand. Remember that certain idioms and figures of speech in English may be unfamiliar or confusing to people who have a different primary language.
- Be aware of nonverbal communication (such as hand gestures) that may have a different meaning to patients from different backgrounds. People also differ in the amount of eye contact, smiling, touching, and physical distance that are comfortable.
Tailoring how you talk with patients can help them better understand the information you are providing. Communicating in a way that makes your patients feel comfortable may help them open up about their health concerns and be more receptive to your guidance.
Providing language assistance in health care settings
Overcoming language barriers is critical for effective patient-provider communication. It allows for mutual understanding, informed decision-making, and better quality of care.
In any type of health care setting, you are likely to encounter patients with a primary language other than English. Here are several ways to support these patients:
- Identify the main languages spoken by your patient population and, whenever possible, match patients with qualified bilingual staff or have other trained medical interpretation services available.
- Start appointments by asking all new patients which language they prefer to speak and read, and whether they would like an interpreter. An “I Speak” card (PDF, 4.6M) can help patients identify their preferred language. Note preferences in their medical records.
- Provide important written materials in your patients’ preferred languages. For example, have office signage, intake and consent forms, prescription labels, and patient instructions available in multiple languages when possible. NIA provides health information for older adults in both English and Spanish as well as links to resources in other languages.
- Maintain a list of referrals to local clinicians and community service providers who speak your patients’ preferred languages, when available.
It can be logistically challenging to provide language assistance services. As a result, some clinicians rely on interpretation by patients’ family members or on bilingual staff members who are untrained in medical interpretation. However, experts strongly discourage this practice. An informal interpreter may be unable to convey medical terminology accurately, may inadvertently misinterpret information, or may be reluctant to share difficult news. Informal interpretation can also interfere with patient privacy.
Using qualified medical interpreters can improve communication, understanding, clinical outcomes, and patient satisfaction with care. Trained interpreters will help ensure that everything said during a medical appointment is relayed accurately and objectively. This checklist (PDF, 207K) provides tips for working with an interpreter.
Providing language assistance isn’t just good medical practice: In some cases, it’s also required by law. Federal policies require health care providers who receive government funds, such as Medicare and Medicaid payments, to make interpretive services and written translations of critical documents available at no cost to people with limited English proficiency. Visit LEP.gov for details about these requirements.
Some states have professional associations and foundations that may provide funding for medical interpreters. Additionally, Medicaid offers reimbursement for some medical interpretation services.
If you are looking for a qualified medical interpreter, the National Board of Certification for Medical Interpreters and the Certification Commission for Healthcare Interpreters have online registries of certified interpreters. The Registry of Interpreters for the Deaf provides a searchable list of certified interpreters in American Sign Language. Many state government websites also provide directories of interpreters and translators to help you locate services in your area.
Tips for culturally sensitive care
How can you work with your patients in a way that respects their diversity? To start, avoid making assumptions about a person’s beliefs, attitudes, or behaviors based on their culture or background. Instead, engage with patients to find out about their individual values and preferences.
Additional ideas for providing culturally sensitive care include:
- Reflect on your own background, beliefs, and values, and consider how they inform your practice. For example, think about your own feelings about aging and how they might influence your interactions with your older patients.
- Get to know the community that you serve. What are the most common racial and ethnic groups? Which languages do they speak? What health, social, and environmental issues do they face? Adapt programs and health care practices so they are appropriate to the groups you serve most often.
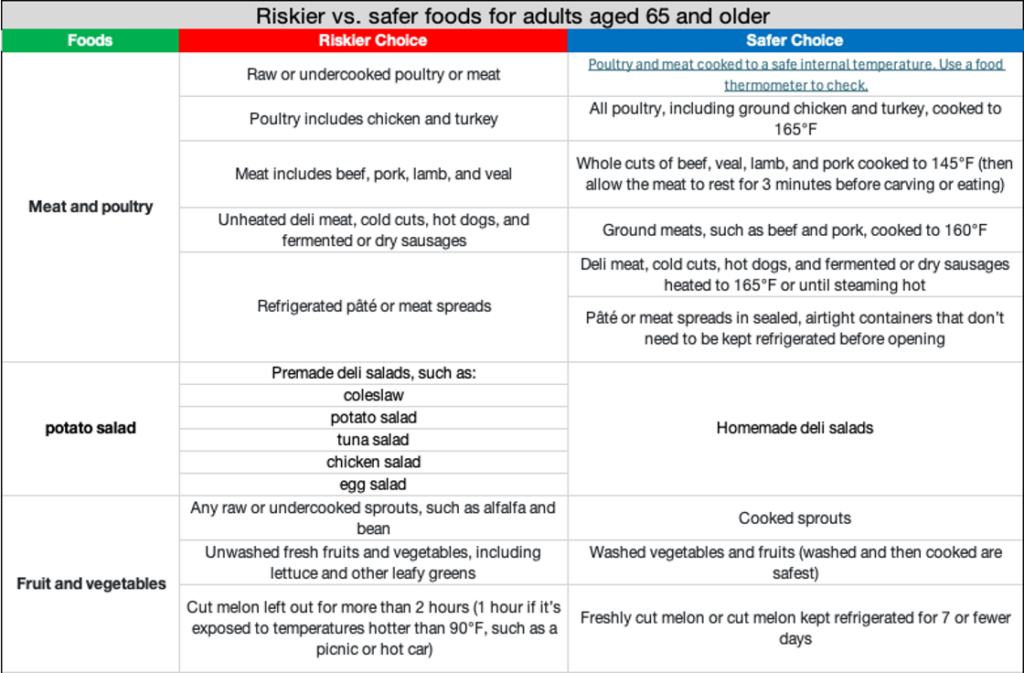
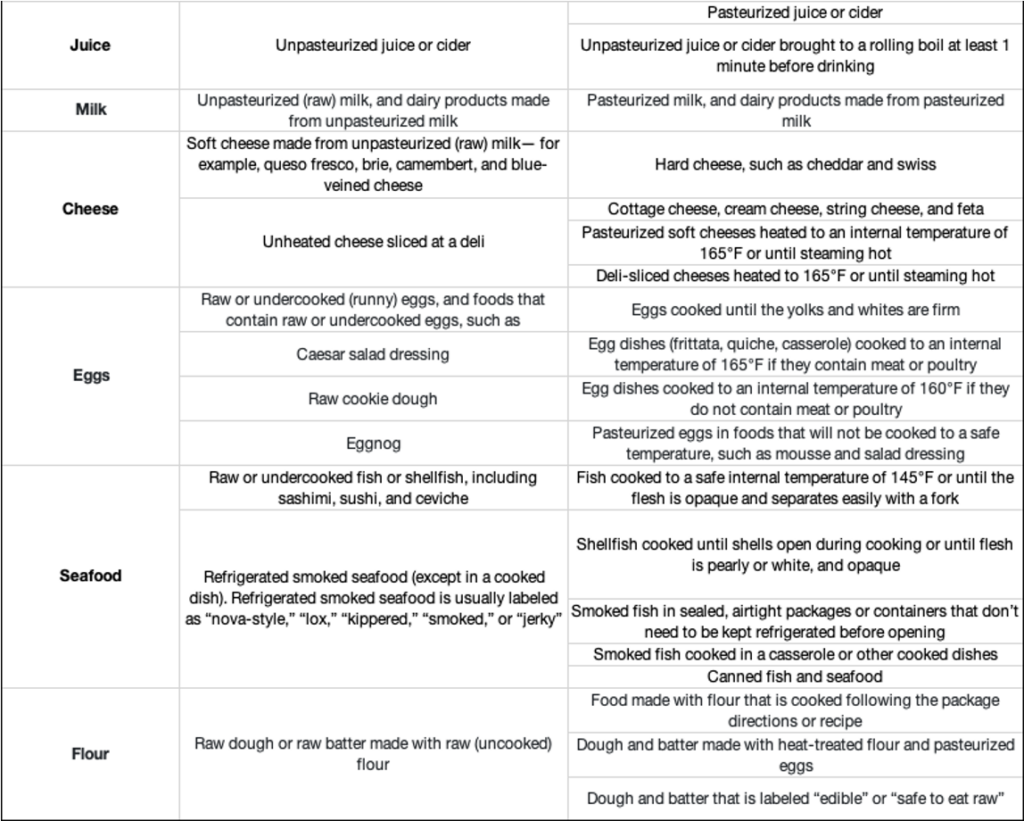
- Recognize that a healthy diet plan may differ among cultural traditions. Patients will have difficulty following dietary advice if it doesn’t take their food preferences and cooking methods into account. The Nutrition.gov Culture and Food page provides nutrition guidance, food options, and recipes from around the world.
- Understand that some patients may value having other family members involved in their health care decisions. Clarify how the patient sees the role of family and any specific information they want shared with relatives.
- For patients nearing the end of life, ask about their health care goals. There may be cultural or religious differences in attitudes toward end-of-life decision-making, such as creating advance directives; disclosing a terminal diagnosis to the sick person or family members; and pursuing life-prolonging treatments, such as a feeding tube.
Different beliefs about aging
People from different cultures and traditions have varied attitudes about aging. For example, in some cultures, older adults are customarily respected for their wisdom and experience. Other cultures tend to be more youth-centered, valuing the qualities of youth over those of old age.
When societies prefer youth over old age, it can lead to ageism. This often underrecognized form of discrimination comprises stereotypes and prejudices directed toward people on the basis of their age. Ageism has serious implications for the health of older people: Studies have associated age-based discrimination with poorer physical and mental health, reduced quality of life, and even earlier death.
Because ageism is so pervasive, it’s easy for well-intentioned health care providers to make assumptions about their older patients and inadvertently reinforce harmful stereotypes. For example, patients and their providers may dismiss otherwise treatable health problems as an inevitable part of aging. As a result, older patients may suffer preventable discomfort and disability.
For tips on avoiding ageism when talking with your patients, see the World Health Organization’s Quick Guide to Avoid Ageism in Communication.
Clinical research needs diversity
It is important for clinical trials and studies to include a diverse range of participants so the results will have broader applicability. Researchers need older adults from many different backgrounds to participate in research so they can learn more about how new drugs, tests, and other interventions will work in diverse populations.
Clinical research also needs scientists from diverse backgrounds, particularly from groups that have been historically underrepresented. Diversity in scientific teams can lead to more creative and innovative thinking, which can help biomedical research represent and benefit people from all backgrounds.
To learn more, please visit https://www.nia.nih.gov/health/health-care-professionals-information/providing-care-diverse-older-adult-population.